

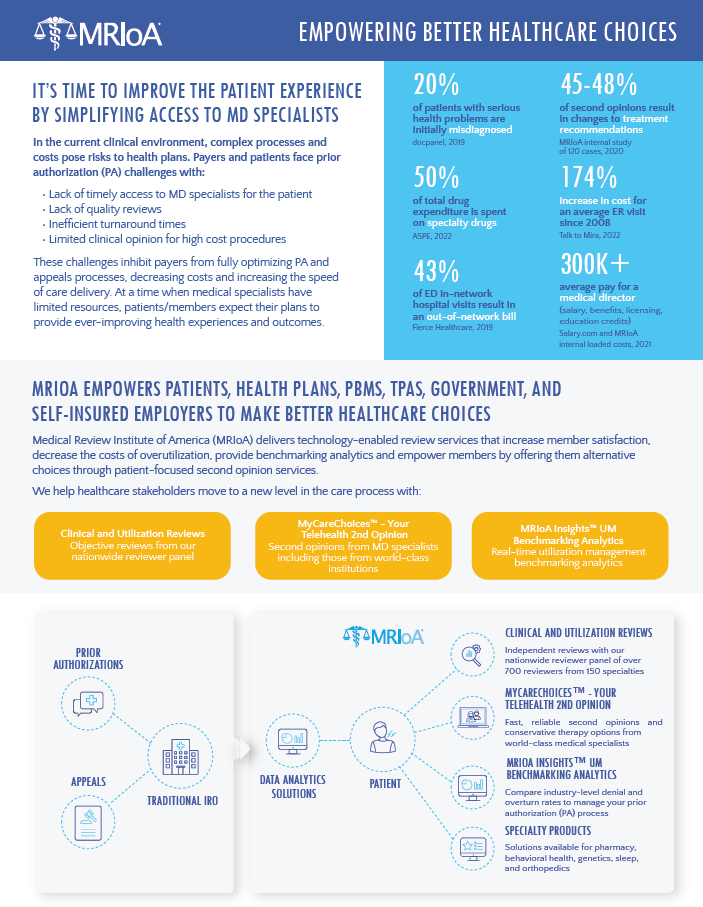
In the current clinical environment, complex processes and costs pose risks to health plans. Payers and patients face prior authorization (PA) challenges with:
These challenges inhibit payers from fully optimizing PA and appeals processes, decreasing costs and increasing the speed of care delivery. At a time when medical specialists have limited resources, patients/members expect their plans to provide ever-improving health experiences and outcomes.